Alzheimer’s and Other Causes of Dementia
Last Christmas, Vicki gave me a dozen handkerchiefs. Now they are gone. Disappeared. Not in the handkerchief drawer or the sock drawer. Not in the clothes hamper. I began to wonder,“ Do I have Alzheimer’s disease?” Probably not. The better explanation for the disappearance of my handkerchiefs—THE HIDERS. The hiders are sneaky. They put pencils behind my ear. They hide my car keys in the refrigerator. They dare to slip my eyeglasses on my face when I’m looking for them. The Hiders are ubiquitous. In every household, they do their dastardly deeds. They are responsible for everything, from lost airplane tickets to the Bermuda Triangle disappearances.
Rather than resulting from senility, our tendency to lose things is more likely due to mindless behavior. Forgetting why we entered a room, saying hello to mannequins, misplacing items—these activities reflect a brain on automatic pilot, which acts without thinking. Almost all of us have seen this mindless behavior in others. A department store clerk will ask you to sign the back of your credit card. After signing the card and the receipt, the clerk holds the receipt next to your credit card to see if the signatures match. Mindless behavior? Did the Hiders climb into the clerk’s skull and conceal her brains? Or does she have Alzheimer’s disease? Doubtful, but these little memory gaps and mindless actions make us wonder, especially as we reach the “senior moments” stage.
Alzheimer’s disease is one of fifty or so medical illnesses that can cause memory impairment and cognitive decline. The all-inclusive term for memory impairment is dementia. About 10% of people with dementia have excessive alcohol intake as the cause of their cognitive decline. Another 10% of people with dementia have vascular causes—small strokes of the brain, cerebral vascular accidents, or malignant hypertension. 20% of dementias are caused by dozens of other illnesses.
An estimated 1.4 million people in the United States have dementia with Lewy Bodies (DLB), a total of 5% to 10% of all dementia cases. Lewy bodies, named for F.H. Lewy, who first described the condition in 1914, result from a buildup of alpha-synuclein protein in neurons in the brain. DLB is associated with dysfunction of the brainstem, limbic, and cortical structures vital to movement and cognition. The severity of symptoms fluctuates over time, with improvements and regressions. However, this dementia will eventually progress to catastrophic disability and death, as with AD. In addition to short-term memory impairment, those with Lewy body dementia demonstrate the following symptoms:
- Judgment, planning, visual impairment
- Balance difficulties
- Hallucinations
- REM sleep disorder
- Disruption in autonomic function—blood pressure, urinary incontinence
Other causes of dementia include Huntington disease with dementia is a progressive inherited breakdown of the central nervous system in early adulthood, affecting movement, cognition, and emotions.
Human immunodeficiency virus (HIV) with dementia is a slow-onset dementia related to the progressive HIV infectious process affecting speed of motion, memory coordination, socialization, affect, and thought processes
Parkinson disease with dementia beginning about one year after the diagnosis of Parkinson disease has been affirmed as dementia with Lewy bodies (DLB) and is characterized by visual hallucinations, motor dyscontrol, and cognitive loss.
Spatio-temporal lobar degeneration (FTLD) is related to a traumatic impact to the frontal lobe, as in a motor vehicle accidents, falls, or a career in football, boxing or similar sports with a repetitive cranial impact
Creutzfeldt-Jakob disease is a degenerative neurologic disorder associated with early development of dementia and the presence of prions, a type of infectious protein
Many reversible conditions can mimic dementia. Specific disorders known to cause pseudodementia include reactions to medications, metabolic disturbances, vision and hearing deficits, nutritional deficiencies, endocrine abnormalities, infections, subdural hematoma, brain tumors, and hydrocephalus, as well as atherosclerosis.
Individuals with dementia require a thorough neurological evaluation to eliminate any treatable causes of memory impairment. A series of relatively inexpensive tests—a urinalysis, complete blood count, metabolic and electrolyte screening, and tests for liver, kidney, thyroid, and adrenal function—identify the most treatable causes of dementia. MRI of the brain can help rule out other causes of dementia.
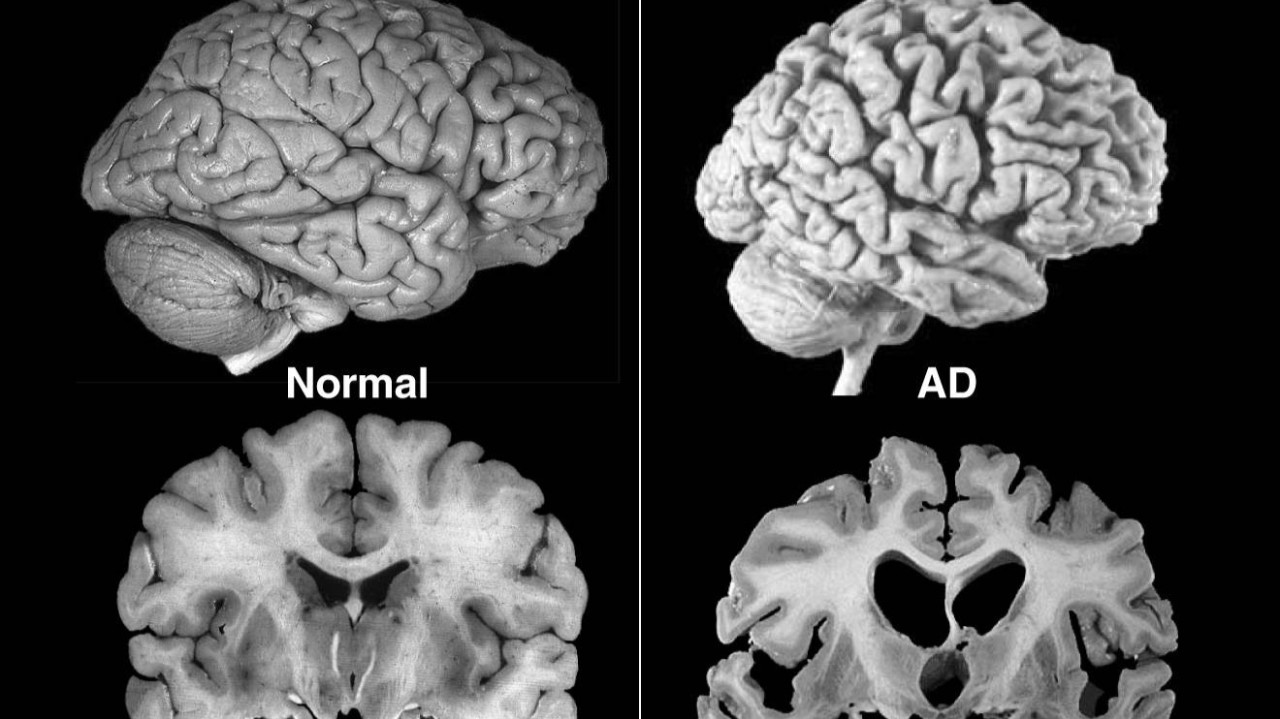
Of all the causes of dementia, Alzheimer’s disease (AD) is the most common. Approximately 60% of people with dementia have Alzheimer’s as the cause of their memory disturbance, a subtle progressive loss of cognitive functioning, with short-term memory loss as its hallmark impairment. The ability to concentrate, make judgments, problem-solve, and engage in abstract thought processes is also impaired.
When, in 1906, Alos Alzheimer identified what he considered a rare progressive neurodegenerative disease marked by microscopic neurofibrillary tangles in the brain, he never conceived that AD would be the most common form of dementia in the elderly and the seventh leading cause of death in the United State
- Between the ages 65-74, 3% will have AD
- After age 65, the risk for AD doubles every five years
- Between the ages 75-84, 19% will develop AD
- For those beyond 85, 47% will have AD
- Over 50% of those over 90 years old show no severe mental deterioration
- Genetic mutations on chromosomes 1, 14, and 21 predict Alzheimer’s before age 60. The ApoE gene on chromosome 19 has been associated with late-onset Alzheimer’s disease. ApoE comes in three forms—ApoE2, ApoE3 and ApoE4. Those who inherit the ApoE4 gene have a greater risk for developing late-onset Alzheimer’s. Two copies of ApoE4 increase the risk of Alzheimer’s disease ten-fold. The majority of patients who inherit the ApoE4 gene fail to develop Alzheimer’s.
Several factors combine with a cascade of events that cause brain cell death in AD. At autopsy, microscopic brain tissue sections reveal amyloid plaques and tau protein tangles. Current research implicates amyloid-beta as a key factor in disease progress. Through complex interactions, amyloid-beta aggregates eventually twist and turn the tau proteins into neuron killers.
Every neuron has an internal support structure partly made up of components called microtubules. These microtubules guide nutrients and molecules from the cell’s body to the ends of the axon and back. Tau stabilizes the microtubules. In Alzheimer’s disease, tau undergoes chemical changes, creating neurofibrillary tangles, disrupting the neuron’s transport system, and leading to neuronal death.
Various inflammatory processes may play a role in the pathology of Alzheimer’s disease. There is growing evidence of a significant interaction between neurons and immunological mechanisms in the brain. Obesity and systemic inflammation can disrupt immunological processes, leading to Alzheimer’s disease progression.
Evidence has accumulated showing that microglia are central players in the mechanism of Alzheimer’s disease. Microglia act as macrophages in the brain, which makes them crucial for clearing amyloid from the brain. Additionally, microglia can be a significant source of pro-inflammatory mediators that may harm neurological function.
Changes in the distribution of brain-derived neurotrophic factor (BDNF) have been reported in Alzheimer’s disease.
There are three stages in the progression of AD. The mild stage can last 2-4 years or longer and include memory loss for recent events, depressed mood, loss of interest in usual activities, trouble remembering names for everyday items, repetition of statements and questions, loss of personal items, personality changes, getting lost, and increasing dependence others.
The moderate stage may last 2-10 years or longer and is characterized by the following:
1. Memory loss for past events
2. Difficulty with simple household chores
3. Neglects personal hygiene
4. Irritable
5. Argumentive
6. Temper outbursts
7. Night-time confusion
8. Wandering at night
9. Delusions and paranoid thinking
10. Requires close supervision
The severe stage generally lasts 1-3 Years. Characteristics include:
1. Difficulty naming parts of the body
2. Unable to recognize family members
3. Loss of social skills
4. Loss of impulse control
5. No frustration tolerance
6. Requires constant supervision
7. Loss of bowel and bladder control
8. Anorexia
9. Severe weight loss
10. Malnutrition
11. Requires total care from others
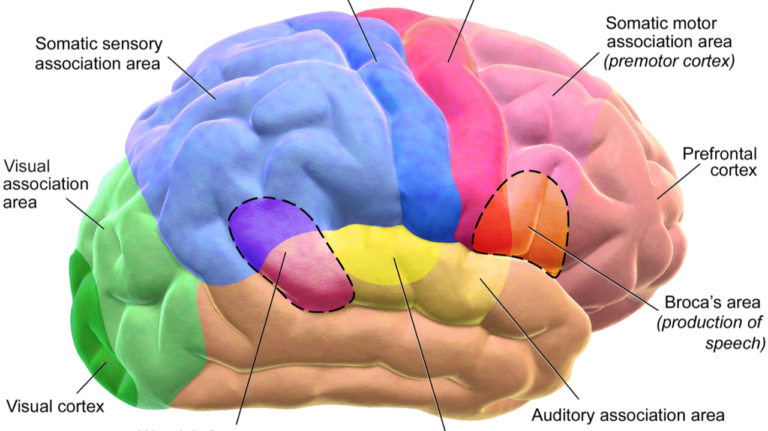
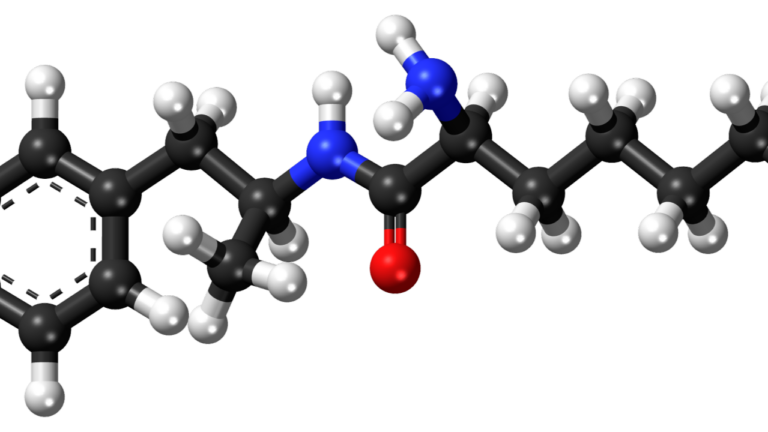
Although no cure for Alzheimer’s exists, several medications slow the development of the disease but do not cure it. Depletion of the chemical messenger acetylcholine seems particularly significant in Alzheimer’s disease. Treatment begins with cholinesterase inhibitors that increase the levels of acetylcholine, resulting in improved neuron transmission. Unfortunately, these medications fail to repair past damage. Instead, they merely slow the development of the disease.
Aricept (donepezil) 5 mg once daily for 4-6 weeks; then 10 mg daily is more helpful in reducing behavior symptoms than improving cognition. Aricept reduces delusions and decreases agitation. It is useless for severe AD. Infrequently, it can cause nausea, diarrhea, anorexia, sleep disturbance, fatigue, and muscle aches.
Exelon (rivastigmine) blocks two enzymes, acetylcholinesterase and butyrylcholinesterase, that cause normal depletion of acetylcholine. During the first few weeks of treatment, 40% of patients may develop nausea, vomiting, or diarrhea. Exelon should be titrated slowly and taken with a full meal to retard GI side defects. If tolerated, the dose can gradually be increased to the maximum dose of 6 mg twice daily. Exelon, like Aricept, slows the progression of AD and is useless for severe AD.
Namenda (memantine) reduces cognitive decline in patients with moderate Alzheimer’s disease by blocking excessive activity of the excitatory neurotransmitter glutamate. Namenda can be gradually increased to 10 mg twice daily. It has been approved to treat moderate to severe AD.
Anti-amyloid monoclonal antibody infusions only work in the early stage of the disease. Donanemab and lecanemab reduce amyloid in the brain. Aducanumab was taken off the market because it was ineffective. These treatments come with a one and eight chance of brain swelling that can lead to hemorrhages. Both donanemab and lecanemab slowed the progression of dementia for only about seven months. Nausea, flu-like symptoms, and headache are common after the treatments. They are costly and time-intensive, with infusions every two weeks for lecanemab and every month for donanemab. The cost, time expended, and risks far outweigh the benefits of this treatment.
Selective serotonin reuptake inhibitors (SSRIs) can help with anxiety, but they’re not adequate for the depressive symptoms of dementia. The gains are very modest, but sertraline and escitalopram have shown benefits. Wellbutrin (bupropion) and Cymbalta (duloxetine) may help alleviate depression associated with AD. The antidepressant, mirtazapine, may reduce anxiety and improve sleep and appetite. Trazodone may reduce agitation, especially in patients who struggle with sleep. Abilify (aripiprazole)and Risperdal (risperidone) may help with agitation, delusions, and hallucinations found in the later stages of AD.
Although we have yet to find a cure for Alzheimer’s disease, we do have some methods to slow down the aging process:
- Stay physically fit. In a study involving 4,600 men and women aged 65 years or older, exercising regularly reduced the chance of developing AD by 30%. A study involving 6,000 women showed that those women who walked at least 10 miles weekly (or 2 miles/5 days a week) reduced their risk of dementia by 30-40%. Exercise stimulates the brain to make new neurons. Regular workouts reduce the risk factors that can lead to AD, including high blood pressure, obesity, diabetes, and stroke. Recent studies also indicate that regular exercise builds brain cell synapses and improves brain blood flow. In addition, exercise causes a boost in endorphins, the “feel good” hormone that enhances mood and memory.
- Train your brain. Spending over two hours a day watching television increases the risk of Alzheimer’s. Instead read. Write. Engage in playing a musical instrument. Learn a foreign language. Memorize Bible verses. Play games like Scrabble, Trivial Pursuit, Scattergories, chess, and Rummikub. Complete crossword or jigsaw puzzles.
- Reduce stress. Stress reduction prevents cell death in the hippocampus, the brain’s memory center. Contemplative prayer, meditation, and yoga are effective stress reducers that can be incorporated into a daily routine schedule. Cultivating friendships also reduces stress.
- Reduce brain shrinkage with a Mediterranean or MIND diet consisting of green, leafy vegetables, whole wheat products, berries, nuts, poultry, and fish, which reduces the risk of developing AD. The risk increases with the number of calories consumed; individuals who consume the most calories double their risk of AD compared to those on a low-calorie diet. Omega-3 fatty acids, known for their antiarrhythmic, antithrombotic, and anti-inflammatory properties, reduce the risks of coronary artery disease, hypertension, and rheumatoid arthritis. They also help guard against depression, bipolar disorder, and AD. Since most “oily” fish are rich in omega-3 fatty acids, the American Heart Association recommends two servings of fish each week. Taking 2400 to 4800 mg of omega-3 fatty acids daily in pill form builds cell membrane phospholipids crucial for neurotransmission.
- Drink 3 ½- 5 ounces of red wine each night. (Baptists can eat red grapes.) Resveratrol, abundant in grape seed and in red wine, is a powerful antioxidant that also dilates arteries by enhancing nitric oxide.
- Supplement the diet with antioxidants. Research has shown that adding vitamins C and E to resveratrol provides a greater degree of brain protection than any of the antioxidants alone because each of these antioxidants scavenge free radicals. Vitamin B12, vitamin B6, and vitamin B9 (folate) break down homocysteine to generate methionine and cystine, antioxidants that increase communication between immune cells. High levels of homocysteine are harmful to the lining of your artery walls, leading to problems like heart attacks or strokes. The following B-vitamin doses are recommended to lower homocysteine levels: 25 milligrams of B6; 400 micrograms of B12; 2.5 milligrams of folic acid
- Take aspirin. Epidemiological studies suggest that anti-inflammatory drugs (NSAID) such as aspirin, ibuprofen, and naproxen prevent brain inflammation that plays an important role in the development of AD. Several studies have shown that long-term NSAID use may reduce the risk of Alzheimer’s disease by as much as 50%.
- Consider estradiol for post–menopausal women. Estrogen docking sites—places where estrogen attaches itself to brain tissue, including the hippocampus—have been identified, indicating estrogen plays a role in memory and cognitive functioning in the brain. Declining levels of estrogen harm language skills, mood, concentration, and attention. Parenthetically, estrogen has a significant role in preventing the development of osteoporosis in women. Because estrogen replacement therapy may increase the risk for heart disease and certain cancers, each woman’s personal and family history must be evaluated before estrogen is prescribed. Most experts recommend the use of natural, soy-based estrogens—estradiol—for replacement therapy because estradiol is the primary type of estrogen made by the ovaries.
- Hydrate. Drink a minimum of 64 ounces of water daily. As a country doctor who practiced in the Big Thicket of East Texas once said, “Most people don’t drink enough water, and their brains shrivel up.”
- Play games that stimulate visual, auditory, and motor skills. Just as keeping a healthy heart requires regular physical exercise, a healthy brain requires regular neuron “workouts.” When brain cells are consistently stimulated, especially in areas involved with language, motor skills, and memory, brain cell death can be slowed.
Aging is a process we all encounter. Most people view it with dread and apprehension, but the prospect of growing old doesn’t have to frighten us. The prevention techniques described above will enable us to cultivate love, joy, and peace that celebrate a well-lived life. And don’t forget humor: he who laughs, lasts. Mark Twain said, “Age is an issue of mind over matter. If you don’t mind, it doesn’t matter.”